What causes autism?
Estimated reading time: 15-20 min
Target audience: Specific audience - Background in medicine/psychology
Update 2021.10.27: A paper outlining the hypothesis has been accepted for publication in Frontiers in Psychiatry (https://doi.org/10.3389/fpsyt.2021.767075)
The potential causes of autism is a hotly debated topic in the public domain, and for a good reason: the increased awareness of autism has led the public to realise that it is a common condition, with pretty much everyone at one point or another coming in contact with an individual with autism. Unfortunately, the public discussion is riddled with misunderstandings and lack of knowledge; something I briefly talked about in this blog post.
I first learned about autism in the psychiatry course during medical school. As someone with an interest in personality psychology and cognitive aspects of behavior, and experience from studying how environmental effects influence brain and behavior development (as a student I investigated how early stress, by being removed from the mother, affected brain development in rats), I created my own understanding of how I thought autism developed, and what it actually was. Throughout the remainder of my medical studies, this understanding crystallised into a concrete model. I did not think too much about this model, though, since I figured it was common knowledge in that field.
Following graduation, I started a Bachelor of Science in child psychology and ended up as a junior doctor in child psychiatry, which eventually lead to a PhD position in child and adolescent psychiatry focusing on – of all possible topics in the world – autism. As I began reading the literature, I realised two things. First, my understanding of autism didn’t seem to be as widespread as I had originally thought. And second, it fit perfectly with the findings from a multitude of previous studies. The hypotheses I developed in my mind, by merely thinking about what autism may be from only the theoretical knowledge of its symptoms and meeting 2-3 individuals with autism, were confirmed time and time again. I also saw that studies often reached the wrong conclusions, or that they struggled to explain their findings. This further stimulated my realisation that I have to formalise and publish this model. I recently published a preprint of a short paper where I outline the basics of the model, which you can read and download by clicking on the image, or here. (Update: I have since published a more extended paper that presents the model in relation to the autism literature).
Below, I will outline an oversimplified explanation, in layman terms, of how that model works. In a later blog post, I will make a more detailed explanation, which will be more suited for those who are doing research on, or working with, autism.
The Three factors that cause autism
Illustration showing the mechanisms involved in the development of autistic behavior, which may in some cases necessitate a diagnosis. Red boxes are risk factors, and green boxes constitute protective factors. Blue and red arrows represent positive/contributory and negative/inhibitory relationships.
I refer to the model as the Pathogenetic Triad (pathogenesis means “the development of disease”), since it consists of three things that together give rise to an autistic behavior:
The Broader Autism Phenotype
Cognitive Capacity
The Neuropathological Burden
This figure illustrates how these three factors interact to cause a behavior which others can identify as autistic, and that a psychiatrist can observe to be severe enough to require a diagnosis of autism.
Below, I will describe each of them, and this figure will make more sense as you read on…
The first factor - The degree of autism-ness
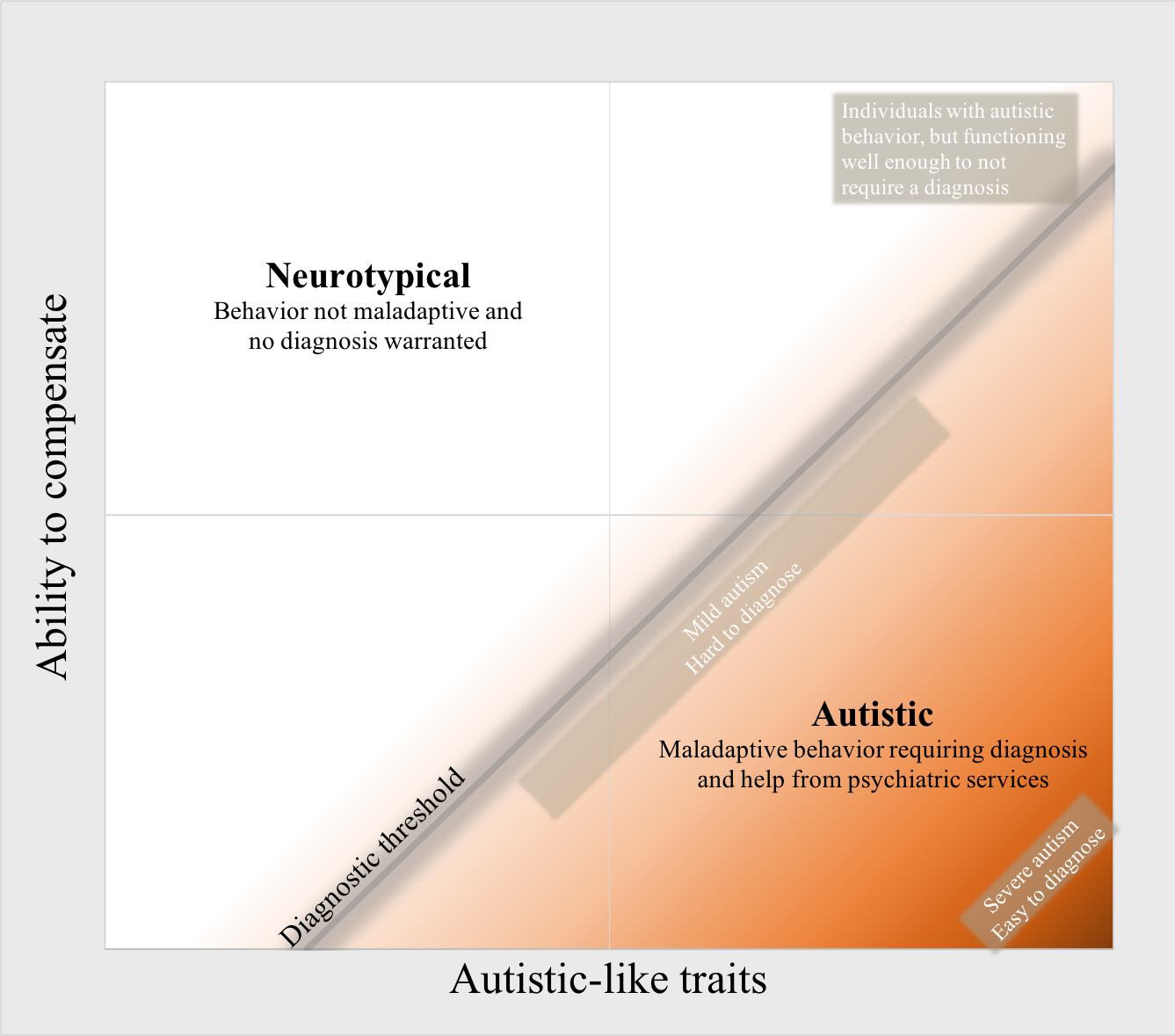
The Broader Autism Phenotype (phenotype here refers to behavior) is a measure of how autistic someone is, irrespective of diagnosis. I believe that the correct way to refer to it is as a personality type. The symptoms that define autism (such as difficulties interpreting social situations, or needing things to be exactly the same or following the same routines every day), are present to some degree in the entire population. These behaviours, or traits, are referred to as autistic-like traits, and everyone has them, more or less. In those with autism, these traits are very strong, and present an obstacle in their daily lives. In everyone else, they are less severe, which does not require a diagnosis; individuals without a diagnosis are referred to as Neurotypical.
The heritability of these traits is high, which is why relatives of those with autism have more traits than others. Also, they are normally distributed, with most people having some traits, and some people having few or many traits. The more of these traits someone has, the more their behavior appears similar to that which we consider to be autism. Unsurprisingly, individuals with autism are disproportionately located at the upper end of the normal distribution of traits. The number of traits has been found to determine the probability that an individual has a diagnosis of autism.
In case you want to test your own autistic-like traits, there are several online tests, such as the one linked here. For reference, the average scores on the linked test are 17.9 for men, 14.9 for women, and 35.2 for those with a diagnosis of autism (published by my friend and colleague Emily Ruzich in this paper).
The second factor - Ability to compensate and adapt
Having many autistic-like traits causes an individual to have a particular set of problems. As with any problems, there are ways to alleviate their impact. If you imagine two individuals throwing a ball as far as possible. One of them is weaker, and will thus have a problem with throwing the ball as far as the stronger individual. However, if the weaker individual has a better throwing technique, either by innate talent or from practicing more, it will be able to throw as far. In other words, one can compensate for low strength with better technique.
The same reasoning applies to the difficulties that arise from an autistic phenotype, such as difficulties in reading social cues. An individual with higher cognitive capacity will be better at interpreting social cues through conscious, and unconscious, analysis. For example, having a higher intelligence will increase the ability of the individual to recognise the pattern that when you first meet someone and they stretch out their arm, this means that they want to shake hands and introduce themselves. An inability to recognise this pattern will cause that social cue to fly right past you. Similarly, an individual with a high working memory (the ability to take in information, keep it in your mind while processing that information, simultaneously taking in more information, and then using the information later on) will be able to listen to what the other person says while planning their own response, perhaps while consciously thinking about why the other person is standing with an outstretched arm. Someone with a low working memory will forget what the other person was saying as soon as they see the other person stretching out their arm, which will make it rather difficult in continuing that social interaction. Similar to the example outlined in the previous paragraph, besides innate cognitive capacity, one can practice reading social cues, and this is a type of therapeutic intervention that has shown good results in autism.
By having a greater ability to process information and recognise patterns in the surroundings, the individual is less likely to appear as having problems, and less likely to be identified as having autism. However, the problems are still there, but they are less visible to other people (and diagnosing psychiatrists). This explains why a delayed diagnosis of autism often leads to problems with depression, anxiety, and exhaustion: to be able to compensate for the problems that occur with strong autistic traits, one must consciously think about, and analyse things that other people unconsciously pick up on, and this is hard work. Females in general have better social skills than males, and since this probably also holds true for those with autism, it may explain why they are not as often identified with autism; the social skills mask the problems that arise from the autistic traits. Instead, they go about life, exhausted from thinking, and confused as to why they seem to be struggling more than others, only to develop secondary mental problems. A better understanding, and earlier diagnosis of females with autism is of great importance, and I will devote a later blog post to this topic.
This diagram illustrates the interaction between the first two factors. The higher the degree of autistic traits, the greater the ability to compensate has to be before requiring a diagnosis. It is the relative difference between these two factors that determines how autistic an individual appears to other people, including diagnosing psychiatrists.
Studies have consistently shown that individuals with autism have lower intelligence and executive functions (working memory is an example of such a function). However, autistic traits and low cognitive capacity are minimally related, and studies indicate that they occur separately from each other. For example, parents that have high cognitive capacity more often have children with mild and high-functioning autism (such as Asperger’s syndrome), while those who themselves have problems with cognitive functions have children with lower-functioning autism. Rather than low cognitive capacity being a characteristic of autism, it may be that individuals with low cognitive capacity and the presence of relatively strong autistic traits experience problems in life, and that they then come to psychiatrists for evaluation. This would indicate that the finding of low intelligence and executive function in autism is not a characteristic of autism itself, but a characteristic of the clinical population with autism, and of our current method of identifying it.
The third factor - Environmental risk factors and the ability to defend against them
There are several aspects to this last factor, the “neuropathological burden”: environmental risk factors raise the risk of autism, largely by inhibiting the development of cognitive capacity, and they do so following an interaction with the immune and autonomic nervous systems. A well-functioning immune system, and a flexible autonomic nervous system, effectively lower the impact that risk factors have on the probability of developing autism. I refer to the resulting negative impact, which all these aspects have, as the neuropathological burden.
The media is always quick to report when some study finds a cause of autism, leading to confusion and fear among the general public. Even within the autism field there is a lingering belief that one might eventually identify a “cause”. If there turns out to be one cause of autism, that would be great, since it would imply a simple disorder and a high likelihood of finding a specific treatment. Unfortunately, I believe this is wishful thinking, based on a misguided medical (simple/categorical) understanding of autism (a clear pathway that is disordered, causing someone to either have a diagnosis or not), when it in fact requires a (complex/dimensional) psychological understanding (a spectrum of behaviours with a multitude of causes and contributing factors). Similar to how personality factors, such as extroversion, do not have one specific cause or biological alteration, neither does autism. Personality factors and complex behaviours have been ever present throughout our evolutionary history, and have been subject to a multitude of selective pressures on different parts of the genome and brain, precluding the existence of a solitary mechanism or cause.
It seems as if everything has been found to cause autism. The use of the word “cause” is rather unfortunate, and they should instead be referred to as “risk factors” since they influence the phenotype and the risk of acquiring a diagnosis. However, not everything can cause autism, and the mere finding that so many and such different mechanisms contribute to autism may be an indicator that they actually inflate the risk of autism indirectly, by influencing something else. That something else may be the cognitive capacity and compensatory ability. Most environmental risk factors that have been shown to cause autism, and other neurodevelopmental disorders, have also been shown to decrease intelligence and executive functions in individuals without causing such disorders. For an overview of studies on these risk factors and their effects, please refer to table 2 and the supplementary material in the linked preprint. Examples of environmental risk factors, or insults, include pregnancy-related complications, autoimmune disorders, infections, medications etc.
Whenever there is something from the environment that affects the body, it shifts the body away from homeostasis (physiological balance) by activating the stress response and/or the immune system. For example, if you get an infection, your body will have to use the energy from the calories you ingest to activate the immune system rather than to make you and your brain grow. During such times, there is less emphasis on continuing normal development, and more focus on regeneration, coping, and survival. This process hinders normal growth processes, and inhibits, among others, brain development over time. The more often you experience the environmental risk factors, and the stronger they are, the greater the effect.
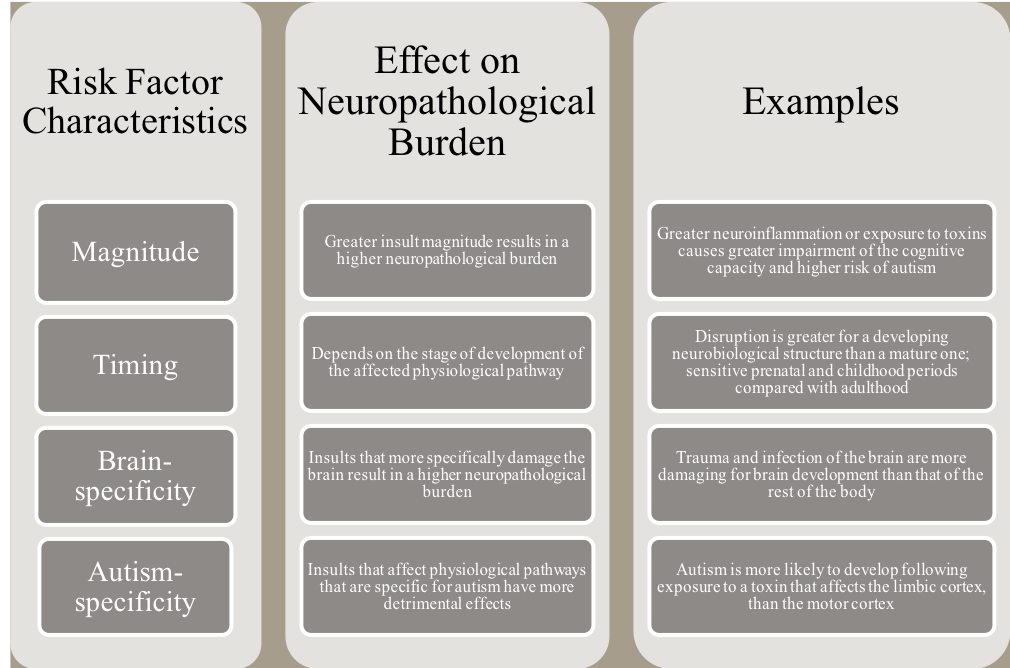
Most risk factors are, like the autistic-like traits, normally distributed. In other words, everyone is exposed to them to some degree. Strong risk factors, such as complications during birth, or the presence of epilepsy, are known to contribute to autism-risk, and it is standard practice to record such things in the medical journals. More subtle risk factors are not accounted for, and have for a long time been thought to have almost negligible effects on brain development. However, their small effects are likely additive and can be detected in particular cognitive domains, such as the higher cognitive functions. The effects of risk factors/insults can be categorised according to their characteristics, which are outlined in the figure to the right.
The higher cognitive functions (such as working memory, intelligence, and even fine motor skills, compared to reaction time, and gross motor skills) rely on the coordination and functioning of several brain areas and multiple, large neural networks. Because of that, any disturbance of the brain’s development will be more likely to negatively affect the higher cognitive functions than the lower cognitive functions. Unfortunately, they are both harder to test, and relatively more important for the compensatory abilities than the lower cognitive functions. So, by experiencing the negative effects from environmental risk factors, the cognitive capacity declines, and this causes the autistic-like traits to become more pronounced due to a lower ability to compensate, learn, and adapt.
Fortunately, these risk factors do not act in isolation, but interact with the body’s defence systems. The efficiency of an individual’s immune system determines how great the damage from each risk factor is. If two individuals get the flu, one may have mild symptoms and recover after 3 days, while the other has severe symptoms for a week. The individual with a better defence against the flu will likely also experience less of the negative effects associated with being sick, since it will sooner return to a state of homeostasis and growth, rather than maintain a state of repair. Many studies have found that immune activation itself is a major risk factor, possibly having greater effects than the diseases themselves, by increasing levels of antibodies and other immunologically active molecules (such as cytokines). Unfortunately, this is why disrupted immune function, such as autoimmune disorders, constitute a risk.
Timely and proper activation of the immune system also depends on the autonomic nervous system, which allocates calories and bodily resources to either growth or repair. Having a flexible autonomic nervous system is of crucial value for optimal development and immune function. This flexibility can be measured using something called Heart Rate Variability (how much the heart rate varies from beat to beat), and the higher it is, the better and faster the autonomic nervous system is at switching back and forth between those two states. Imagine two individuals getting scared by a snake. An individual with a flexible autonomic system will get a rush of adrenaline, which will inhibit their ability to rest and digest and grow, and also their ability to think and make judgements. But very quickly they will return to a calm homeostatic state. An individual with an inflexible system will remain in that adrenaline-driven phase for much longer, delaying proper growth and development. An individual with low heart rate variability that lives in a psychologically stressful environment, is often sick, or experiences many of the above-mentioned risk factors, will spend a relatively shorter time in homeostasis and much less of their bodily resources will be used for development of body and brain, compared with an individual with high variability. This leads to a lower cognitive capacity, and a higher risk of autism.
Finally, I have to note that many studies have found not only lower cognitive capacity in autism, but immune and autonomic dysfunction (with some scientists even arguing that it is an autoimmune disorder). I would instead argue for the fact that these findings are due to a sampling bias. The individuals that have a strong autistic phenotype, and that also happen to have an immune dysfunction, will be more likely to come to a clinic. Due to this sampling bias, many of the findings in the autism field are not findings specific for autism itself, but for a clinical population (the disorder, rather than the phenomenon of autism). This is underscored by the fact that many similar disorders (such as schizophrenia) also have findings of immune and autonomic dysfunction and low cognitive capacity. If we want to study autism per se, and not “patients” in general, we must first have a theoretical framework that correctly explains autism, and then parse out the effects of the other contributing mechanisms. This is the reason behind my personal research interest in the broader autism phenotype, which I believe is at the heart of autism, and should be investigated neurobiologically much more than it is today.
Implications of hypothesis
· All three factors have high degrees of heritability, explaining why autism is consistently found to be one of the most, if not the most, heritable condition within psychiatry.
· All of them are also normally distributed, which contributes to the complexity and many facets of observed behavior; there is not a binary label where you are either text-book autistic or you are not, but an intricate interaction causing a spectrum of behaviors. This situation, where you have many different presentations, is called “heterogeneity”, and is a standing issue in the autism-field. This hypothesis explains why there is heterogeneity (the environmental insults cause different patterns in the structure and function of the brain, leading to different behavioural phenotypes), and proposes a way to make autism less heterogenous (by characterising the insults and categorising study participants accordingly, and including both subtle and severe insults in the clinical evaluation). On a side note, identification and measurement of subtle insults are immensely difficult, and that is the reason why I suggest heart rate variability as a surrogate measure. This may capture enough of the individual variability in a person’s exposure to past insults so as to be clinically useful. I will explain how and why in a future blog post.
· This framework suggests a sampling bias in the clinical population (with regard to cognitive, immune, and autonomic function), which would have serious implications for how research findings are interpreted, and how studies should be planned. When investigating the degree of autism-ness, one should include undiagnosed individuals with high and low degrees of autistic-like traits; when investigating the causes behind getting an ASD diagnosis, one should include individuals with high degrees of autistic-like traits, with and without a diagnosis. Otherwise the findings will be confounded by the investigation of two or three separate factors, and not only one which is assumed (autism vs. neurotypical).
· It explains why there is a sex ratio difference in autism. In all three factors of the triad there are sex differences. First, testosterone increases the autistic-like traits, which is why males have a stronger broader autism phenotype. Second, females have a higher social intelligence in several cognitive domains; a double-edged sword that will partly alleviate the social difficulties from the autistic phenotype, and partly camouflage their autistic behavior, decreasing the probability of being clinically identified and receiving a diagnosis. Third, females are less biologically vulnerable, and environmental insults often affect them less than they do males, which causes a lower neuropathological burden in females and lower autism risk (for example, due to a stronger immune function, they also have a higher rate of autoimmune disorders).
· There have been several case studies published of individuals without previous autistic behaviors, that following environmental insults (such as infections) developed a full-blown clinical picture of autism. These findings have remained unexplained, since autism is supposed to be a condition that is present at birth, and does not develop after the first few years of life. Within this framework, the neuropathological burden, and specifically the autism-specificity characteristic of an insult, explains how someone can develop autism even in adulthood (or at least an autistic-like disorder). For example, by damage to fronto-temporal areas, which are important for compensatory working memory and other higher cognitive functions, or by damage to areas underlying key social functions, such as Theory of Mind (the ability to understand the thoughts and intentions of another person), the behavior of the person will appear more autistic.
This image illustrates why studies find that individuals with low intelligence and executive function more often have several diagnoses, compared to those with a normal/high cognitive capacity. The image presents an individual with a particular personality (such as a lot of autistic traits, but very few schizotypal traits, represented by blue lines on the right and left in the illustrated normal distribution). It also presents two scenarios, in which the individual has experienced a lot of environmental risk factors and has a low cognitive capacity, and vice versa. In the first scenario, illustrated by the left red line, the individual shows several maladaptive behaviours that require diagnoses and psychiatric help (the intensities of the personalities are located to the right of the threshold/red line). In the second, the individual only gets diagnosed with autism, since it has a lot of only those traits. The higher the neuropathological burden (NB) and the lower the cognitive capacity (CC), the farther to the left the diagnostic threshold (red line) moves. And any behavioural phenotype that the individual has relatively a lot of (to the right of the diagnostic threshold) will become a problem. This hypothesis is presented as a framework for neurodevelopmental disorders, but could also be a framework for any behavioural problem (such as personality disorders, where the first triad factor is represented by personality domains such as extroversion, narcissism etc.).
· Lastly, the framework explains why different disorders co-occur, and why studies find that it is more common for individuals with low cognitive capacity to have more numerous diagnoses. Basically, a higher neuropathological burden and lower cognitive capacity will cause a behavioral phenotype to become maladaptive at lower levels. Autism, ADHD, OCD, etc., can all be explained through this framework, and each of them have an underlying “broader phenotype”/personality that is normally distributed. Each such phenotype for a person will be at a different level on the normal distribution, with strong traits being relatively infrequent. An individual with a low neuropathological burden and high cognitive capacity, will be rather unlikely to have more than one phenotype that is at the upper extreme end of the spectrum. Refer to the illustration and caption below it for a more detailed explanation.
If you have any thoughts or comments, let me know in the comments-section below, or send a message through the contact-form.